Admitting that we are wrong is painful. We try to avoid it. Research shows that before changing our minds, most of us will search for a way to dismiss evidence that runs counter to our beliefs, especially if we have voiced these beliefs to others.
There are good reasons why we are like this – reasons that relate to social bonding and status. But when trying to co-ordinate the public response to this pandemic, mental rigidity is a problem. This unprecedented challenge requires us to learn and adapt as we go. We need to open our minds to emerging evidence if, as a society, we are to respond well.
In such circumstances, there is no shame in being wrong. I was wrong about willingness to wear masks. Because early guidance was ambiguous and few people initially wore them, I thought there was little chance the Irish public would take to masks voluntarily. Evidence proved me incorrect: the proportion of customers wearing masks in shops increased to a majority well before they were mandatory.
Do people just tell researchers that they comply to make themselves look better? It seems not
We need to generate and pay attention to behavioural as well as medical evidence because, for now, behaviour is our primary defence against the virus. However, current behavioural evidence suggests that many people, including people in influential positions, hold beliefs that are probably wrong.
This article describes some evidence and makes constructive suggestions for how we might use the findings to galvanise public support to fight the virus. The findings come from multiple studies, mostly undertaken by Amárach Research, UCD, or my team at the Economic and Social Research Institute (ESRI).
Complacency and fatigue
Let us start with the constant assertions that the population has become complacent and fatigued, leading to an inevitable fall in compliance with guidelines and support for restrictions. Even the World Health Organisation published advice this week on tackling “pandemic fatigue”, which it defined as “demotivation to follow recommended protective behaviours, emerging gradually over time and affected by a number of emotions, experiences and perceptions”.
First, notice that complacency and fatigue are not natural bedfellows. Complacency is not associated with tiredness, but comfort. Second, even if some of us experience either feeling – I am certainly tired of this virus – it does not necessarily drive our behaviour.
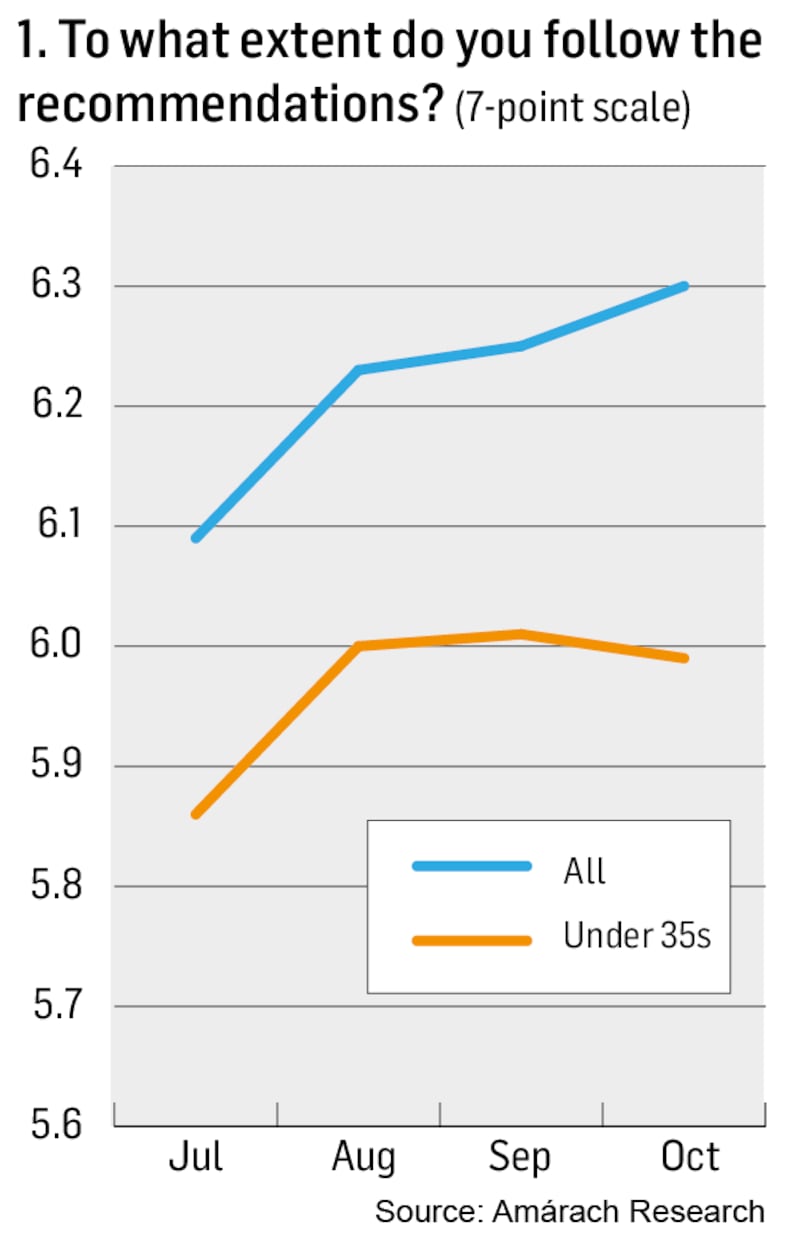
The evidence? Amárach’s tracking survey records that compliance with public health guidance in Ireland since July has not decreased, but increased (Chart 1).
Now, if you are like most people I talk to, your mind has just protested that this cannot possibly be true and searched for reasons to doubt the survey. Do people just tell researchers that they comply to make themselves look better? It seems not, because not only do people report that they themselves are following guidance more since July, they report that other people are too (Chart 2).
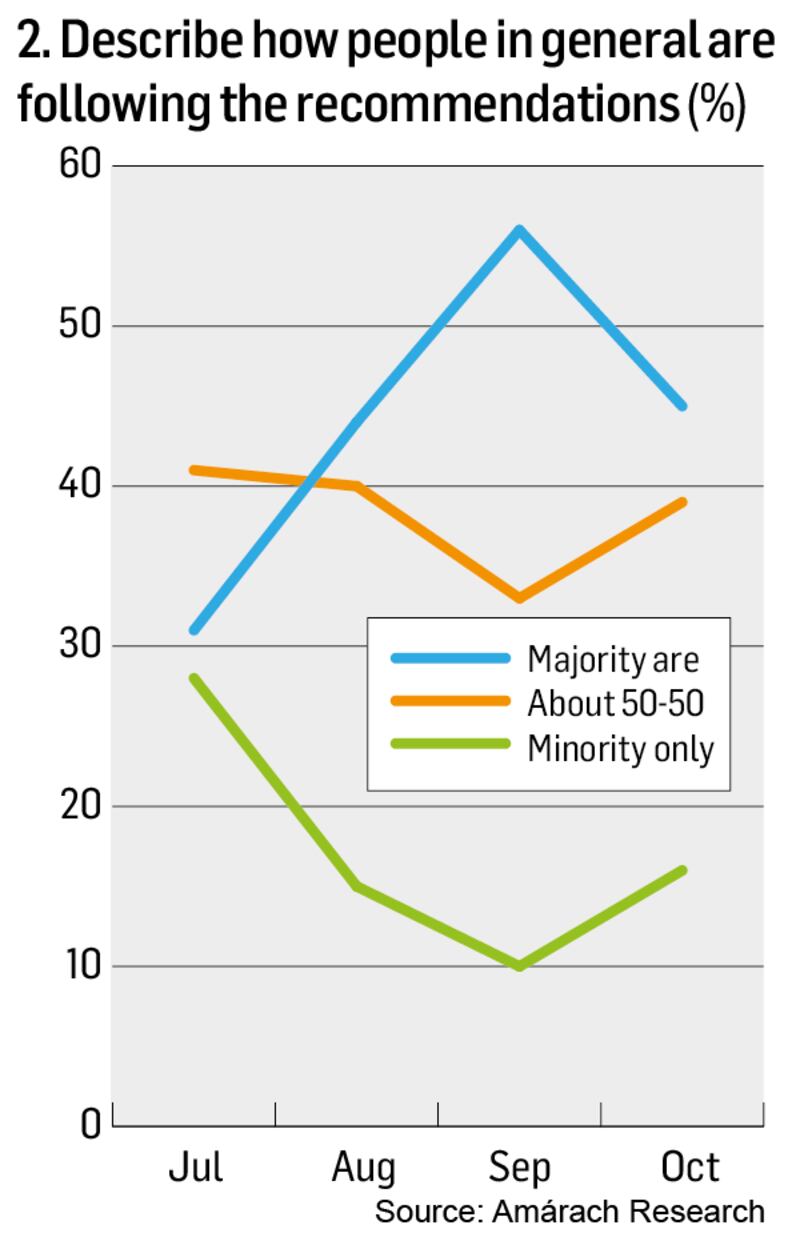
Still think the survey must be dodgy? Try this. When you look closely, the patterns over time make sense. Reported compliance matches measures of motivations from multiple studies. People worry a lot about catching the virus and, in particular, giving it to others. As infections fell in early summer, so did worry and reported compliance. As we rapidly lifted restrictions and the virus began to spread again, worry increased and so did reported compliance.
The patterns reflect another influence: social and economic opportunity. When the pubs recently reopened and young people went back to college, while overall reported compliance continued to go up, it fell marginally among young people. Perceptions of compliance by others fell, too, but remained well above July levels.
Ah yes, you might think, but what about young people? Haven’t they stopped caring? No. While our studies record lower compliance among under-35s, this is not because they don’t care. Most worry about catching and passing on the virus, but when trading off risk against social opportunities they push the boundaries – doubtless more so after a drink.
After the Government accelerated the lifting of restrictions back in June, the population increasingly began to worry that we were going too fast
This is unsurprising. Multiple data sources show that younger adults have endured the biggest hit to mental wellbeing. On top of disproportionate income loss and unemployment, their social and relationship lives have been largely taken away. They report anxiety, low mood and boredom. When opportunities arise, temptation is higher.
So the shape of the data over time does not reflect inevitable impacts of tiredness or complacency, but an active trade-off. People balance perceptions of risk to themselves and others against much wanted opportunities to socialise and earn money.
Support for restrictions
Data on support for restrictions tell a similar tale (Chart 3). After the Government accelerated the lifting of restrictions back in June, the population increasingly began to worry that we were going too fast.
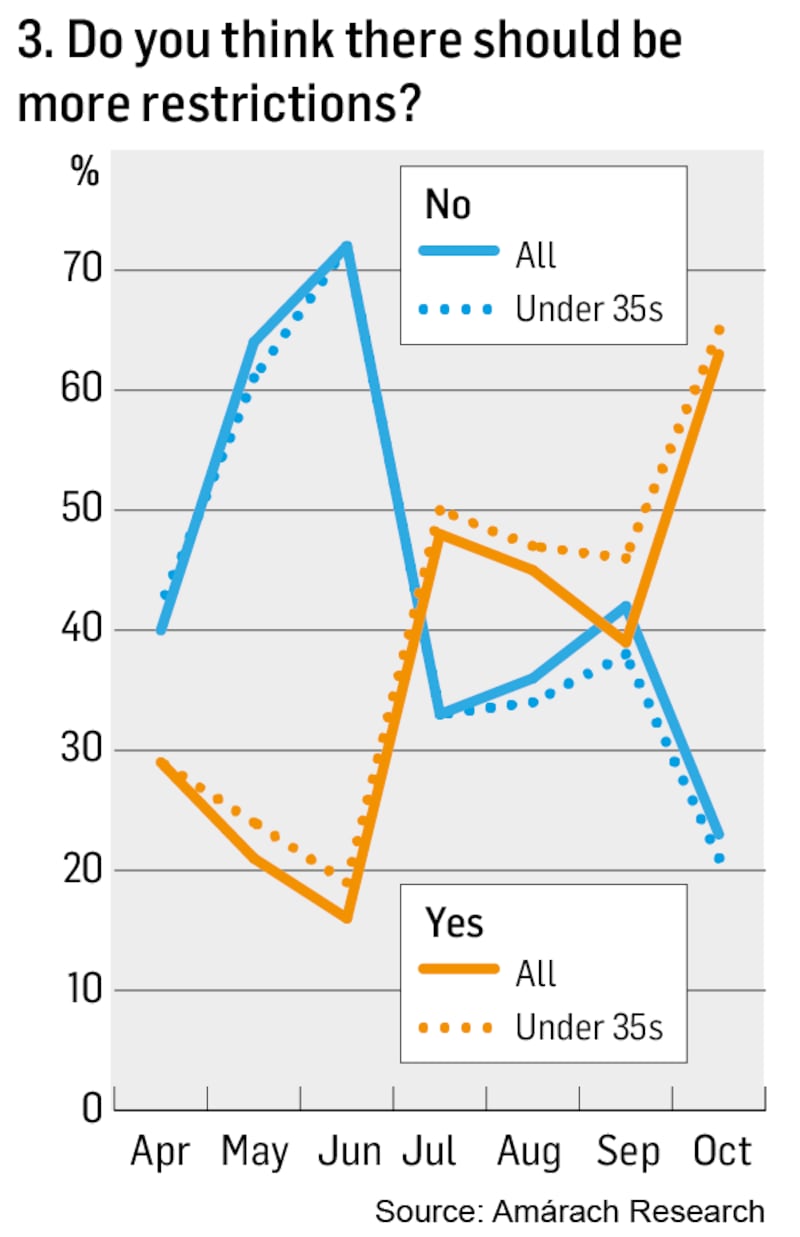
Just before the latest move to Level 3, 63 per cent wanted more restrictions, compared with 23 per cent who did not. Interestingly, support for more restrictions is even bigger among younger people. Parents of teenagers and young adults will know well that young people can both want more rules and be more inclined to break them.
Overall, the evidence suggests that complacency and fatigue are not primary behavioural influences, at least not in Ireland. Far from giving up, we are up for the fight. Furthermore, looking at the balance of evidence, I suspect that the overwhelming focus on compliance is blinding us to some less palatable lessons.
Blaming others is a more comfortable psychological state than facing our own challenges.
Consider the recent sharp rise and subsequent fall in infections in Kildare, Laois and Offaly. Did compliance with guidelines suddenly and dramatically fall and then rise in these counties? Almost certainly not. Infection rose and fell because changes in the rules altered opportunities for social and economic interaction. The primary influence on behaviour was the level of permissible gathering.
I need to be cautious here – I am a behavioural scientist not an infectious disease expert – but between the behavioural and medical science, a misperception may be operating. A thought experiment makes the point.
Suppose one night this week I meet a friend outside a pub. The tables are a bit too close together and we stay a bit too long: the kind of noncompliance we have all seen. Assume this doubles my chance of infection compared with keeping to time in a place that’s more safely laid out.
We underestimate inherent risk in repeated compliant behaviour, underestimate the risk reduction associated with getting outdoors, and are too slow to call the doctor
Here is the issue: I am still less likely to catch the virus than someone who follows guidelines perfectly but meets a different friend on three separate occasions.
This is true simply by the laws of probability, but evidence shows that people don’t reason this way. We are inclined instead to think in binary terms: behaviour is either safe or not. This raises an important research question: does the rate of infection respond more to changes in levels of compliance, or to changes in the amount of compliant socialising?
I have seen no evidence that answers this question, but I know people are happier to discuss the former than the latter.
Let’s go outside
Even among those who are complying, perception and understanding matter. Behavioural data from our lab highlights two specific lessons.
First, while the population has absorbed the main risk factors well, there is one they underestimate: the reduction in risk when you meet people outdoors rather than indoors.
Second, too many people will delay calling the doctor when they first feel a symptom. They are inclined instead to wait and see how things develop, in part because they worry about being blamed for poor behaviour.
To summarise, we have useful behavioural evidence – though we should be collecting more. It suggests that we trade off perceived risk against the desire to maintain social and economic activity. Younger people are no different; they simply find it harder.
Meanwhile, some perceptions are not accurate. We underestimate inherent risk in repeated compliant behaviour, underestimate the risk reduction associated with getting outdoors, and are too slow to call the doctor.
Given this evidence, what needs to be done?
For a start, we should stop fretting about complacency and fatigue, because they are a misdiagnosis of our psychological condition. Instead, good communication needs to focus on helping people to negotiate the trade-off between risk and maintaining enough of their social and economic life to get by. This trade-off might be shifted in multiple ways.
Walk with coffee, with those you care about and with those who care about you
Anything we can do to help people to cope will reduce the temptation to take risks. This means fewer negative messages about bad behaviour and more positive messages about looking after our wellbeing. We need encouragement, not disparagement; to urge people to do what they can do safely, rather than focus on what they cannot.
A simple example. Data suggests that getting outside makes us happier. So encouraging people to buy good clothing and wherever possible socialise outdoors both hits this mark and allows us to keep talking about how meeting outdoors reduces risk.
Don’t just meet for coffee, walk with coffee.
By the way, the more we do, the more coffee our beleaguered cafes with their limited outdoor tables will sell. Evidence also suggests that wellbeing can be improved by focusing more on the relationships that matter to us most.
Walk with coffee, with those you care about and with those who care about you.
Clearly, the trade-off we face is more acute for young adults. We need to stop putting our energy into criticising them and demanding punishment and, instead, put it into discussing, devising and implementing safer social opportunities.
This doesn’t just mean “working with student bodies”, it means putting effort and resources into organising safe social gatherings and activities, preferably outdoors. We need to use the full range of organisations, including workplaces, colleges, sport clubs, cultural centres and youth clubs to do what they can. We should be prepared to provide public funding for good ideas and to spread them.
Simple messages
Despite criticism of complex Government communication, there have been positive recent developments. Behavioural science shows that simple messages are more likely to alter behaviour.
Advice to halve social contacts compared with the week before is much simpler than urging compliance with restrictions that must be looked up online because they differ from sector to sector. Simpler messages can be combined with more positive encouragement about safely enjoying those social contacts.
Behavioural evidence shows that narrative is often more persuasive than statistical arguments. So it is good to see that the Department of Health has begun to release anonymised stories. A recent one about a couple whose behaviour led to multiple infections caught the imagination and was the most-read item on multiple news outlets.
More could have been said, for the story showed not only how rapidly the virus can spread among those with highly active social lives, but that it can spread among those who are complying with guidelines indoors. Stories impart understanding and can be used not only to warn, but to encourage.
We are, of course, tired of this virus, but our behaviour nevertheless reflects renewed attempts to negotiate unpleasant trade-offs and to stay happy.
We need ideas and encouragement.
Dr Pete Lunn is a behavioural economist with the Economic and Social Research Institute. He is also a member of a subgroup that has advised the National Public Health Emergency Team (NPHET) on the public response to the pandemic







