Numbers can illuminate, or numbers can confuse. The true scale of Covid-19 deaths is contested globally. Equally so in Ireland, where mortality rates put the State high on some tables, and low on others.
What is at the heart of a big problem with Covid-19 data?
Yes, there is a dazzling array of colour-coded interactive maps, amazing diagrams showing that disease curve, and brilliantly illustrative graphics. Often, however, they cause confusion and political friction.
Confronted by a mountain of constantly updating data, it is extremely challenging for a non-specialist to get an accurate read on the Covid-19 pandemic. Accuracy is the issue.
Without complete data, comparisons between countries cannot be entirely valid, whether for cases, test numbers or deaths. League tables, however, always create a temptation to make judgments.
The problems are compounded by different countries being at different stages of dealing with the virus: the rising (exponential) phase, the flattening the curve stage, and the declining cases/deaths phase.
Why does accuracy matter?
Having data that can be relied upon is critical. Properly done, it helps to restrict spread, to identify clusters, to inform doctors and politicians about where problems will come, and when.
Now, accurate data, not opinions, is needed to guide the route out of lockdown, minimising the risks of a second wave of coronavirus coming in the autumn, or later.
Equally, accurate data is required to persuade people to make difficult decisions about their own lifestyles, and to stick with them even when boredom and frustration has set in.
Yet statistics are rarely perfect, especially in complex field of public health. So it becomes an exercise in probability, an evaluation of risk. It is not about producing perfect accuracy.
DCU professor of health systems Anthony Staines points to the big ongoing argument in the United States about people dying from coronavirus and dying with coronavirus.
If a person becomes seriously ill from Covid-19, gets kidney disease, and dies – while another is already dying and gets the disease, “the last little kick” provided by Covid-19 can push them over the edge.
“Everybody dies because their heart stops but that is not recorded as a cardiac death,” he adds. So when it comes to Covid-19, doctors know how to weigh up contributory factors and direct cause of death.
So what exactly is the problem with Covid-19 mortality rates?
Covid deaths have been subjected to distortions: some inadvertent; others deliberate. In the early stages of the pandemic, health services were overwhelmed, deaths were reported late – rates were clearly under-stated.
Some countries used different counting rules. Some counted Covid-19 deaths only if people died of it in hospitals, others excluded Covid-19 if there were serious underlying conditions.
Governments are always sensitive about international league tables, but they are even more prickly when it comes to Covid-19 mortality league tables, if they are featuring in the lower rungs.
"You don't need to be a genius to understand why Boris Johnson has ceased to publish details of how well Britain is doing compared to the rest of the Europe," the Guardian's economics editor Larry Elliott noted.
The accuracy of the UK’s numbers improved once the Office for National Statistics began issuing daily figures including deaths outside of hospitals, especially where Covid-19 was mentioned on the death certificate as a factor.
Russian deaths could be 60 per cent higher than reported because health authorities are only including deaths of coronavirus-positive patients if pathologists said the virus directly caused death.
Distortion came in the form of nationalist leaders such as Donald Trump and Brazilian president Jair Bolsonaro suppressing figures for propaganda purposes; insisting they had control of things.
Repeatedly, the US president claimed falsely that cases were inflated. The opposite was true. People who died at home or in a long-term care facility without making it to the hospital were initially not counted as Covid-19 deaths.
Moreover, the US’s community cases were much higher than reported, due to inadequate testing, while large numbers of people were dying at home without a doctor in attendance.
Many deaths were simply listed as “respiratory failure”, “pneumonia” or “multisystem organ failure”. This happened elsewhere, too, especially in the early stages where the virus was circulating unknown to anyone.
The true picture will take a year to emerge. Only then will it be truly known which countries backed the wrong horse by relying too much on herd immunity or less-aggressive testing and tracing.
It will also become clear if Sweden’s less restrictive approach will be considered enlightened or misguided. It had the highest coronavirus death rate in the world per capita over the past week after continuing to shun lockdown.
How should we read Irish Covid-19 death rates?
Let’s address the confusing, apparently bad indications first.
On "deaths per million", the Republic of Ireland is ranked at eighth in the world with 330 (as of May 25th); worse than US and Brazil. However, when it is based on deaths per 100,000, Ireland is in tenth place, with 31.9 cases.
Yet, if a "case fatality rate" measurement is used – the proportion of deaths compared to the total number of people diagnosed with Covid-19 for a certain period of time – Ireland stands at 29th place with 6.4 per cent. [https://www.statista.com/statistics/1104709/coronavirus-deaths-worldwide-per-million-inhabitants/]
Ireland is among the top 10 EU countries for all Covid-19 deaths. But if only deaths in hospitals are counted, then Ireland falls to 13th. Currently, Ireland is among the world’s worst for deaths in nursing homes.
But the data coming from other countries is clearly suspect, so most comparisons are invalid. [https://coronavirus.jhu.edu/data/mortality] Death tolls are influenced by the speed of the virus's spread, along with different reporting and testing rules. "Data sources may use country figures related to cases and populations recorded at different points in time," the Department of Health explains.
Putting those inevitable contradictions aside, Ireland has always followed detailed WHO guidance and advice from the European Centre for Disease Prevention and Control.
A death due to Covid-19, for example, “may not be attributed to another disease [such as cancer] and should be counted independently of pre-existing conditions that are suspected of triggering a severe case of Covid-19”.
Many countries are continuing to ignore deaths outside hospitals, says Staines. The UK wanted the lowest possible number reported. “Other countries were downright worse; they have told fairy tales,” he declared.
Undercounting is happening globally. “Excess deaths” – above and beyond what we would have expected to see under “normal” conditions – are about double official Covid-19 death counts.
So are Irish death rates reliable?
In short, yes, but with caveats. From the outset, NPHET reported all Covid-19 laboratory-confirmed deaths, in both hospital and community settings, unlike other countries that reported hospital deaths only.
In mid-April, Ireland broadened mortality reporting and included “probable” Covid-19 deaths as well as laboratory-confirmed ones, in line with changing WHO guidance.
However, registrations of deaths in Ireland can take three months. At one point, chief medical officer Dr Tony Holohan asked for quicker reporting in the interests of accuracy.
A mortality paper prepared by NPHET concludes mortality in Ireland "has been within the lower range in overall terms compared with other health systems across Europe".
In 11 countries where it is possible to adjust for population density, Ireland ranks third lowest and has a markedly lower mortality curve than the three highest-ranked countries (Spain, France and Italy).
What indicates reliability?
Writing in publicpolicy.ie, Dr Patrick Malone at UCD's Geary Institute analysed the actual and estimated number of Covid-19 deaths, concluding that Ireland's figures are robust, with reconcilable limitations.
During March and April, the daily number of new deaths rose steadily, peaking at 70 deaths in mid-April. “The exceptional number of deaths on April 24th was due to the inclusion of 185 ‘probable’ deaths to the official figures on this date,” wrote Dr Malone. “These represent deaths where a laboratory test has not been done but where a doctor believes a death is associated with Covid-19.”
Since then, the daily toll has fallen. However, the statistics clearly illustrated the pain felt in nursing homes and community residential centres, which have become the epicentre of the pandemic, not hospitals.
Confirming the reality, chief medical officer Dr Tony Holohan reported on May 18th that residential care clusters had jumped to 459. Of these, 258 had happened in nursing homes.
Residential care facilities accounted for 6,190 cases; 4,820 of these in nursing homes. Some 62.6 per cent of all Covid-19 deaths (969) were associated with residential care settings; 54.5 per cent (843) occurred in nursing homes alone.
When there is an inquiry – which is likely, given the scale of deaths, and in the interests of finding what we did right and what we got wrong – these will be the terrible statistics that tell much of the story.
Where does independent analysis on RIP.ie come in?
Under the State's regulations, deaths must be reported to the General Register Office within three months, which is slow by international standards. Ireland's official mortality statistics were last published in June.
"This is a very long window compared to other countries," says UCC economist Seamus Coffey, "That led me to wondering whether the RIP.ie website could serve as an informal real-time proxy of mortality for Ireland."

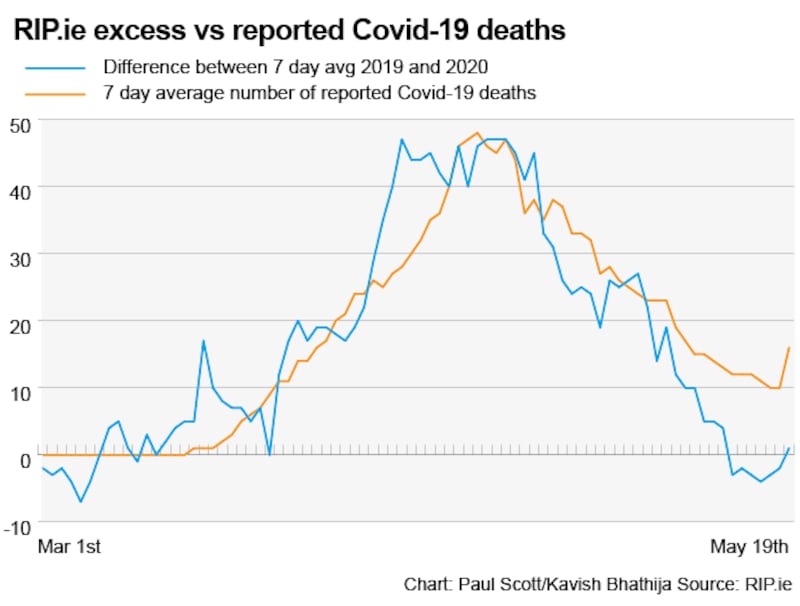
The RIP.ie figures are “a good proxy” for overall mortality, he believes, and show that official preliminary figures “are likely capturing close to the full extent of Covid-19 deaths in the country”.
“April 2020 was a particularly bad month for mortality since modern records began in 1960; it was the worst April in that period. 2020 now has more deaths than recent years,” Coffey adds.
And it can be believed that Covid-19 is responsible for the excess deaths because the number of excess deaths and the number of Covid-19 deaths are not so far apart, even allowing for the delay in registering deaths.
“Ireland has been reporting every death. The data is reliable; you can hang your hat on them [the figures],” says Staines, who highlights the “astronomical number of excess deaths” that have taken place in the UK.
Though not perfect, the Irish data offers reliable indicators. In his view, though, the numbers argue for a full-scale attempt to “crush” Covid-19, not just to contain it.
So, is there a better way to get a snapshot of Covid-19 deaths?
Financial Times data analyst John Burn-Murdoch says deaths-per-head tables are misleading, "because it tends to make smaller countries look like they are doing worse". Ireland clearly falls into that category.
Instead, he developed “an excess mortality tracker” that compares a country’s excess deaths and differences between mortality rates this year and previously.
The tracker revealed the UK had 54,000 more deaths than usual in March and April compared to 30,000 reported Covid-19 deaths at the time. His numbers this week prompted Spain to revise its own figures.
Applying the excess deaths standard, how should we to read differences between Northern Ireland and the Republic?
Comparing Covid-19 death rates north and south of the Border is a statistical minefield. It prompted social policy specialist Prof Mike Tomlinson to crunch the data and conclude Northern Ireland fatalities are "well above" those in the Republic – by the order of 41 to 50 per cent.
This prompted a sharp war of words in Northern Ireland. A casual comparison of “official” figures – deaths per million population – would suggest the Republic’s rate was much higher than the North’s.
Northern Ireland Statistics and Research Agency data showed there were 599 excess deaths for the North by May 8th. While there are no comparable details for the South, he turned to Coffey's RIP.ie analysis.
“Coffey has shown that there is a remarkably close relationship between the official count of registered deaths and RIP.ie notices going back over five years,” Tomlinson notes.
What is revealed when you dig deeper on comparisons between the UK and Ireland?
Fully accepting the pitfalls that exist with international league tables, Dr Rory Dwyer, a critical care consultant at Beaumont Hospital, has, however, drawn other lessons from the numbers.
His analysis of raw figures from the Health Protection Surveillance Centre and figures from a UK audit indicate that 23 per cent of patients in Irish ICU wards died, compared to 46 per cent in the UK.
The median age is the same in both countries – 60 years. So were the same type of patients “equally sick”? Dr Dwyer looked at ventilator numbers. Again, the differences are stark: 33 per cent (Ireland) mortality to 58 per cent (UK).
Trying to explain the gap, Dwyer believes Irish ICU units were not overwhelmed, though some came close. “It was really because of lockdown, and everybody geared up and was able to cope with what arrived.”
In the meantime, Dr Patrick Malone believes timely data on excess deaths, clusters and outbreaks are “very useful information in making crucial decisions about opening up the economy and in lifting restrictions”.
When will there be total clarity on Irish Covid-19 deaths?
The real measure of higher mortality during this time will be in figures from the Central Statistics Office later this year. They will take into account all deaths registered.
By then, detailed international numbers and the true human cost of the pandemic will be known. Politicians and countries that made wrong choices will be exposed. However, those same numbers will also offer lessons for the future.












