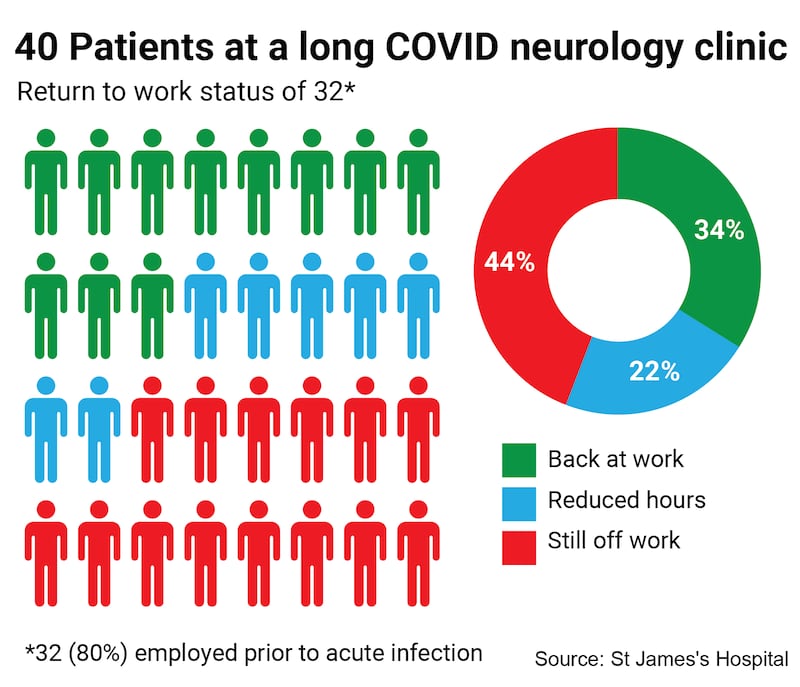
Most of the patients attending the State’s only neurology clinic for long Covid sufferers have yet to return to work fully, a year and more after they were infected, a seminar on the condition has heard.
Of the 40 patients attending the clinic, 80 per cent were working before they contracted Covid-19. Just 34 per cent of these have returned to work, while 44 per cent are off work at least a year later and 22 per cent are on reduced hours, according to Dr Aoife Laffan, consultant neurologist at St James’s Hospital.
Fatigue and cognitive concerns, migraine, mental health struggles and functional neurological disorder (FND) were the main reasons cited for not returning to work. FND refers to disorders caused by an abnormality in brain signalling with no significant structural damage in the brain.
‘Genuine disorder’
The clinic has begun taking referrals for post-Covid vaccine symptoms, she said, and has seen four patients so far. All have a diagnosis of FND and the three who were working before the pandemic have yet to return to it.
Ninety per cent of the patients attending the clinic are women with a median age of 45 years, Dr Laffan told the online seminar on tackling long Covid, organised by the Policy Forum for Ireland.
One in five patients attending the clinic has FND, which is often triggered by an illness or injury, she said. “It is not a diagnosis of exclusion, or a psychological dismissal of symptoms or another way of telling patients their symptoms are all in their head. It is a very real and genuine disorder whose symptoms are internationally recognised.”
The path back to work can be supported through phased returns, adapted roles and the option of working from home, she said.
Many people with severe complications had actually had a mild original infection, she said.
Although six long Covid clinics have been established countrywide, these are led by infectious diseases consultants. Patients that fail to recover are often referred to neurology or psychiatry.
There is one neurologist treating the condition nationally, she said. Ireland has one neurologist per 45,000 people, compared to a European average of one per 10,000 people. There are more than 23,000 people on the neurology waiting list.
Infectious diseases consultant Prof Jack Lambert said it was known from early 2021 that brain effects were a significant issue in the treatment of coronavirus. Of the first 100 virus patients treated in the Mater, about one-quarter had fatigue and/or headaches.
One-fifth of participants in one Irish study had signs of depression a year after infection and 72 per cent had concerning alcohol use, added Prof Lambert.
“The research suggests between 10 and 30 per cent [of] Covid patients develop life-limiting conditions, primarily neurological and neuropsychiatric in nature, and these conditions can persist for years.”
About 150,000 people in Ireland have long Covid, Prof Daniel Altmann of Imperial College London told the seminar, extrapolating his estimate from UK surveys.
There, he said, the number of sufferers is plateauing, even though people are “triply vaccinated” and milder variants are circulating. Even though the risk posed by newer variants is 40 per cent lower, there are many new cases of long Covid because so many re-infections are occurring.
“People are not getting better fast. There is a growing burden of unhappy, unwell patients who don’t feel they are getting [the] best care,” said Prof Altmann.
WRC case
Phil Ní Sheaghdha, general secretary of the Irish Nurses and Midwives Organisation (INMO), said Ireland was out of step with the rest of Europe in not treating long Covid as an occupational injury.
For many healthcare staff, long Covid has been a “catastrophic event”. Some are “on their way to retirement in their 30s” while for others from outside Ireland, their right of residency is threatened by the lack of protections.
“Many are having to fund enormous out-of-pocket expenses on private physiotherapy and rehabilitation. Yet if they weren’t healthcare workers, many wouldn’t be in this situation.”
The INMO and other unions have been campaigning to have long Covid designated as an occupational injury; their case is due to be heard at the Workplace Relations Commission shortly.
!['People are not getting better fast. There is a growing burden of unhappy, unwell patients who don’t feel they are getting [the] best care.' File photograph: EPA](https://www.irishtimes.com/resizer/v2/KTSEOFONWJDSZJXAA6SR35KF5A.jpg?auth=268dd841e629eec22e47e7d382fc55c588d94ce9ea105e588f0193028860c590&smart=true&width=1024&height=681)




